
The procedure to be taken when a tick bites can vary significantly depending on the specific circumstances of the incident. Sometimes the parasite is simply removed from the skin and thrown out, but in other cases it should be carefully removed from the skin alive, placed in a tightly closed container, processed in the wound at the bite site, and then hurry to the medical institution together with the saved parasite.
Such differences in actions are due to the fact that in different situations the danger of a tick bite is not the same. For example, in regions endemic for tick-borne encephalitis or Lyme borreliosis, people need to do everything possible to minimize the risk of serious consequences from infection. Sometimes it is quite troublesome, but any time spent in this case is justified.
Next, we will step by step consider the tactics that should be followed when detecting a sucked tick on the body. If competently and in time to remove the parasite itself, as well as implement a number of preventive measures, then even in the most unfavorable situation, the chances of facing serious complications after a tick bite will be minimal ...
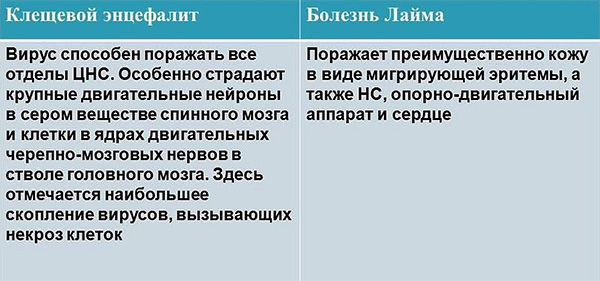
How tick bites are dangerous and why they require special attention
The main reason why bites ixodic ticks much greater importance is attached than, for example, the bites of bedbugs, fleas or mosquitoes - this is the ability of certain individuals of these parasites to infect humans with deadly diseases: tick-borne encephalitis, borreliosis, spotted fever and some others.

Tick-borne encephalitis (TBE) is considered to be the most terrible disease, since it is much more often than all the others, it leads to the development of disability (usually associated with mental disorders) and deaths. In addition, the causative agent of TBE is a viral infection, against which today there are no specific drugs and which, because of this, is more difficult to treat.
Borreliosis Lyme is known for its high prevalence worldwide.If you violate the rules of diagnosis and treatment, it can also lead to disability and death, but with the right approach to dealing with it, it can be treated fairly quickly and successfully.
On a note
Other tick-borne infections (at least in Eurasia) are much more rare, and deaths during their development are rare. On the one hand, due to this, they are considered less significant, on the other - it is precisely in the fact that they are given less importance and their deceit is hidden. They are rarely consulted by doctors in time, medical errors are more frequent, resulting in severe illness and, as a result, complications.
See also article How to distinguish an encephalitic tick from a normal (non-infectious) parasite.
It is important to understand that in some cases a person may die or become permanently disabled by the effects of a tick bite., and in almost any region, even one in which no tick-borne encephalitis is noted - from the same borreliosis, for example. The chances of not becoming infected at all or of easily moving the disease are high, but even a small probability of a threat to life justifies quite troublesome measures that need to be done after a tick bite.
The first step is to immediately remove the tick.
It is necessary to understand that if the tick has not yet been stuck, but is only found crawling through the body in search of the place of attachment, then it can simply be brushed away. It is not dangerous and is not fraught with infection. The danger is precisely the tick bite, that is, when there is a violation of the integrity of the human skin, followed by bloodsucking.

It is also possible that a tick is detected directly at the time of cutting through the skin - when it has formally bitten, but has not yet stuck. There is a short period during which the oral apparatus of the parasite, although it is in the skin, does not yet emit saliva into the wound. Consequently, the infection has not yet occurred.
However, in practice, it is impossible to understand whether the tick has already isolated infected saliva in the wound, and it is pointless to speculate in this situation. Therefore, it is recommended to assume that if the tick has already pierced the skin, then he could easily transmit the infection.
On a note
Some experts believe that the risk of infection is less likely if an encephalitic tick was removed during the first 24 hours after suction, and greatly increased if the parasite lasted more than 48 hours in the skin.Such data are not without logic, since the intensity of the supply and exchange of fluids between the parasite and the host increases precisely by the middle of the insertion period.

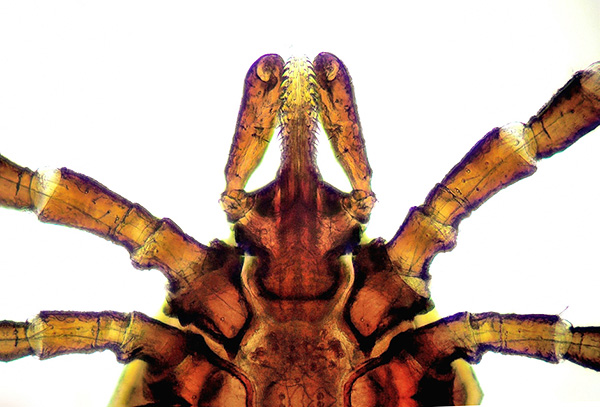
If the tick has already sucked, removing it without some skill is not so easy. Certain difficulties are associated with several factors:
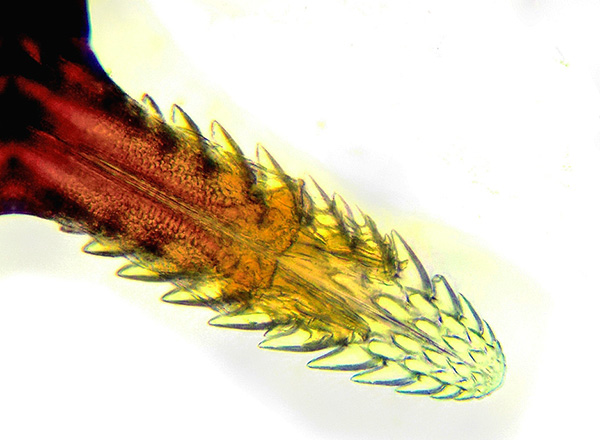
- Ticks are able to hold very tightly in the host’s skin (see how the tick bites and what happens). The parasite burst the skin at the site of the bite with its jaws, and in many species a cement sheath of hardened saliva is formed around the proboscis (which has many notches), which very rigidly fixes the parasite. As a result, it is often easier to break a tick's body than to tear its mouthparts from the skin. However, such a development can not be allowed - the parasite should be removed entirely;
- At tick removal it is impossible to squeeze his body, pierce or stretch it, because with all such manipulations the parasite releases additional portions of saliva (possibly infected) into the wound.
The photos below show a proboscis mite dotted with notches:
In many cases, another factor complicating the extraction of a tick is the man’s fear of this procedure.In practice, due to inexperience, many people can prepare for this action for half an hour, smear the parasite with oil, try burning it with alcohol, etc. And all this time, the bloodsucker continues to secrete its saliva under the skin, possibly - along with infectious agents.
Therefore, the first rule: speed is important when removing a tick. If the choice is between pulling out a tick for a second with tweezers, and smearing the parasite with kerosene, and then waiting for two hours when he finally suffocates and unhooks himself (this, by the way, will not happen), then it is better to simply pull out .
Actually, this is exactly what experienced tourists, fishermen and hunters do. When an experienced man sees a mite, he immediately grabs it with his nails under the body, right next to the skin, and pulls it out. If a head remains in the skin, it is immediately removed with a needle, like a splinter.
It takes 2-3 seconds to remove the tick, another minute to remove the head from the skin. At the same time, the head itself remains very rarely in the skin - in one case out of several hundred bites, and if this happens, it is no longer an infectious hazard, since all the glands that release infected fluids remain in the parasite's severed torso.

On a note
Partly, precisely because of the rarity of head seizure, many hunters find it inappropriate to buy and carry with them special tick makers. If an experienced person bites 10-15 ticks in one season, then in a few years he may have a situation once that the parasite's head remains in the skin. Moreover, this situation is identical to the danger of splinters getting under the skin.
A person who encounters a tick for the first or second time in his life is better to remove a stuck parasite with the help of special devices. Such devices are not designed for pulling out, but for twisting the parasite - it is during the rotation of the gnatosome that the fixation of the oral organs in the cement case weakens, after which the bloodsucker does not even need to be pulled, since it disappears by itself.
These twisting devices include:
- Tick Twister, Trixie Tick Remover and similar hook extractors. They are very simple, inexpensive and easy to use;

- Tongs in the form of special tweezers;

- Extractor spoon, on the "scoop" which is a small slit, which captures the tick for further unscrewing;

- Special lasso handles in which a loop of fishing line is pounced on the tick, is tightened, and then the parasite is twisted out with a twisting motion;

- Handles with tweezers at the end, and the forceps unclenched when you press the cap, and when released they are compressed. Ticks are gripped with forceps and rotated;

- Flat wrenches-keys, convenient for carrying in a wallet, but less convenient for extracting parasites than hooks.

Also, the simplest tick maker can be done independently - at home or in nature. For example, a flat wooden stick with a wedge-shaped slot at the end allows the parasite to be effectively unscrewed like an industrially produced tongs.
The removal of the tick itself is as follows:
- The extractor is slit under the mite and rests against it so that the edges of the incision are pressed tightly against the body of the parasite and fix it;
- The device begins to rotate in an arbitrary direction around the axis of the body of the parasite (it does not matter, which way to unscrew the tick - clockwise or against). As a result, the tick begins to rotate with the twisting;
- After 2-3 revolutions the parasite usually falls out by itself. If this does not happen, you can make another 2-3 turns in the same direction and try to pull the tool up smoothly and easily. If the parasite is not removed, the sequence is repeated again - it is scrolled 2-3 full turns, then slightly pulled.

On a note
Both at home and in nature, it is convenient to use a regular thread - a loop is made on it and pounces on the head of the tick under its body. Then it is tightened around the head at the point of contact of the body of the parasite with the skin. After that, the ends of the thread twist one around the other with a rubbing motion of the fingers. At a certain point, the body of the tick, which will fall out of the skin after a few revolutions, will begin to rotate with them.

If there are no devices at all, you can pick up the bloodsucker with your nails under your torso, try to squeeze the head (without squeezing the body itself), make rotational movements in one and the other side to loosen the proboscis and then smoothly pull it out of the skin.
What not to do when removing a tick:
- It is impossible to squeeze the body of the bitten parasite with tools or fingers. When pressure is applied to the wound, additional portions of saliva are squeezed out, which is undesirable;
- It is impossible to leave a tick in the skin for a long time - the longer the parasite sucks blood, the higher the risk of infection of a person with an infection;
- You can not pour oil on a tick, cauterize it, put gadgets on it with kerosene or a repellent with the expectation that it will detach itself. It will not be detached: it will either be completely saturated in a few days and only then it will be unstuck, or it will die right in the skin. In the latter case, it will still have to be deleted, only already dead.
If, however, the mouth organs of the bloodsucker (they look like a small black dot in the center of the wound) remain in the skin, they can be easily removed with a simple needle or nail scissors - just like a splinter is removed.
What to do with the parasite immediately after removal
After removing the tick from the skin, further actions are based on the risk of developing a tick infection:
- If it is known that the area is not endemic for tick-borne encephalitis and Lyme borreliosis, then the tick is usually thrown away;
- If the area is endemic to CE, but the bitten one has tick-borne encephalitis vaccinationthen the tick is again thrown away. If there is no vaccination, the parasite is saved for further analysis.

Above all, the risk of tick-borne encephalitis is taken into account. A tick is not always tested for infection by borrelia (although it is useful to do this) - emergency prevention of borreliosis is not carried out, and the disease itself, if it develops, is relatively easy to treat (it is only important to monitor your well-being in order to recognize anxious symptoms in time,which will be discussed below).
See also more about borreliosis ticks and the effects of their bites.
On a note
It is possible for complacency to hand over the tick to the analysis of infection with pathogens of borreliosis - if the pathogen is not detected, then there will be no cause for concern.
If the tick needs to be preserved, it is placed in any hermetically sealed container, a wet cotton wool is put in there and carefully sealed. It is desirable that the parasite was alive and unharmed, but even if it was crushed or torn apart during extraction, its remains should also be preserved - they are quite suitable for analysis.

Then, as quickly as possible, the tick must be delivered to the laboratory for research. There they will be able to identify whether the parasite is infected with an infection.
The next step is competent disinfection of the wound.
Immediately after removing the tick, the bite site should be treated with an antiseptic solution - for example, an alcoholic solution of iodine, green paint, hydrogen peroxide, miramistin or chlorhexidine (in extreme cases, just alcohol or vodka). This will not prevent tick-borne infection, but protects against secondary infection by bacteria that may be on the skin and get into the wound.

Bandages and glue the bite with a plaster is not required.Almost never a wound bleeds, but it can itch and itch. If the tick has had time to get enough, independently to unhook and crawl away, the wound in the form of a dot at the puncture site of the skin will have a characteristic appearance, which will make it easy to distinguish the tick bite, for example, from a mosquito bite.
You can not try to squeeze the blood or blood from the wound - it will not help to remove the infection if it got there, but will only contribute to the accelerated spread of pathogens into nearby tissues. Also, do not cauterize the bite site or pick it up in order to pour the antiseptic inside.
If a red spot appears on the site of the bite, it hurts or itches badly - anesthetic ointment is usually used (Menovazan, Lidocaine, Fenistil-gel). When rashes and allergies appear, the skin is treated with Advantan, suprapin is given to the injured person (in rare cases hospitalization may be required, especially if the child has signs of urticaria).

Thus, first aid for a tick bite does not imply the administration of any powerful antiviral agents or antibiotics. After the PMP does not require any special care for the wound: you can wash,you can wet the bite with water and keep it in the sun - it will not have any effect on the condition of the victim.
Analysis of tick infection
It is advisable to check the tick for infection with an infection, if only in case of a negative result, to completely remove concerns about the risk of infection. However, even if the tick was infected, this does not at all mean that the bitten person will certainly get sick - that is, a positive test result is not a reason to start treatment.
The tick is tested for tick-borne encephalitis virus infection in microbiological laboratories at various hospitals and clinics, as well as in commercial laboratories. In each city, you can get the address of such a laboratory in the reference or by the emergency number.

The study of a tick usually lasts 2-3 days and costs about 500-700 rubles. The analysis is carried out in the event that the tick was delivered for inspection no later than the third day after the bite.
Mites before analysis do not need to freeze, alcoholize and try to feed something. It is enough to place it in a hermetically sealed container with a piece of wet cotton.
Moreover, if the bite occurred in an endemic region, and the medical institution has drugs for emergency prevention of tick-borne encephalitis, then the victim is likely to immediately hold it - in case the tick turns out to be encephalitic.
On a note
Emergency prevention of tick-borne encephalitis by introducing immunoglobulin is effective only in the first 4 days after the bite. After this time, the procedure no longer makes sense.
If, according to the results of the study, the tick was a carrier of tick-borne encephalitis virus, then it is necessary to closely monitor the condition of the victim for at least a month. In addition, 2 weeks after the bite, blood should be donated to detect tick-borne encephalitis antibodies. To pass tests before 10 days is meaningless, since the result will certainly be negative (antibodies will not have time to form in sufficient concentration).
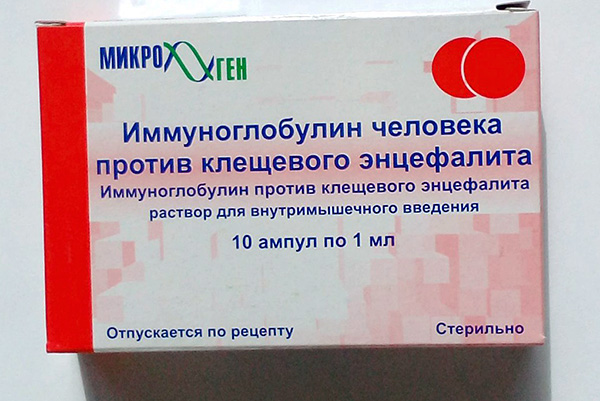
Emergency prevention of tick-borne encephalitis
Emergency prevention of tick-borne encephalitis is the introduction into the body of the affected serum with antibodies to the virus-causative agent of the disease. These antibodies (immunoglobulins, or otherwise - gamma globulins) bind viral particles and prevent them from spreading and replicating in the body.If such prophylaxis is carried out before the beginning of active reproduction of viruses, then the disease will not develop.
On a note
However, it is worth noting that the effectiveness of such preventive measures has not been proven by methods of modern evidence-based medicine in the West. Accordingly, neither in Europe nor in the United States do they carry out such prophylaxis of TBE. In Russia, immunoglobulin preparations against tick-borne encephalitis are considered effective, and the method of emergency prophylaxis is used in all regions endemic for this disease.
The main requirement for such prevention is to conduct it in the first 4 days after the bite. It is believed that in the first 2 days its effectiveness is maximum, for the 3-4 day it is already significantly lower, and starting from the 5th day it makes no sense to do it.
All preparations of immunoglobulins for emergency prophylaxis of CE are produced in Russia, the most common production serum Microgen. Packaging it costs about 6500-7000 rubles for 10 ampoules of 1 ml. The amount of the drug is calculated according to the body mass of a person: for every 10 kg of body weight, 1 ml of the product. Accordingly, it is possible to calculate the approximate cost of the injection (the procedures themselves, without taking into account the cost of the immunoglobulin, are either free of charge in the polyclinics or there are symbolic money).
Immunoglobulin injections against CE are not performed during pregnancy and lactation.
A few words about the means for self-prevention of tick-borne encephalitis
Contrary to common misconception, self-prevention of tick-borne encephalitis with pills or traditional medicine is impossible after a bite. This is due to the fact that effective means for such protection do not exist today, and those that are commercially available are either empty-case or preparations with unproven efficacy.
An example of a useless drug is Anaferon, a widely known homeopathic remedy that does not contain components that could somehow affect the development of infection.
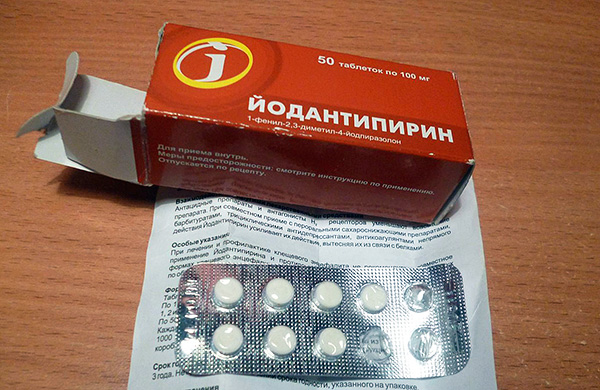
Drugs with unproven efficacy are Yodantipirin and Remantadin. Their ability to inhibit the development of tick-borne encephalitis has not been confirmed by evidence-based medicine (which, however, does not prevent a large number of doctors from prescribing these drugs as prophylactic).
Other drugs that are marketed as antiviral or immunomodulatory (for example, Reaferon-Lipint, Cycloferon) also have no influence on the development of the disease.
On a note
Similarly, there is no independent prevention of borreliosis.Borreliosis itself is successfully treated with relatively inexpensive, affordable and safe antibiotics (the drug of first choice is doxycycline). Theoretically, antibiotics could also be used for prophylaxis, but in practice their use would be required for almost everyone bitten because of the wide range of borrelia themselves, despite the fact that the actual infection rate is low and approximately comparable to the frequency of side effects from the antibiotic itself. In other words, it is simpler and safer to not carry out medical prophylaxis, but to treat borreliosis itself during its development (as revealed by a blood test for borreliosis).
Monitoring the condition of the victim after a bite: what to look for
Regardless of the fact that emergency prevention of tick-borne encephalitis, as well as the region in which the person was bitten and whether he had anti-encephalitis vaccine, after tick bite, you should carefully monitor the victim’s condition for at least a month, and if symptoms of the disease appear to the doctor.

On a note
A tick can infect a person with various infections, so the presence of tick-borne encephalitis vaccination is not a complete protection.
Average tick-borne encephalitis incubation period and Lyme borreliosis is 1-2 weeks, but can sometimes stretch up to several months. If at this time the victim's condition worsens or the symptoms listed below appear, then this is a reason to consult a doctor as soon as possible for a prompt diagnosis. The alarming symptoms after a tick bite include:
- Fever with fever up to 38-39 ° C;
- Pain in the head and muscles;
- Convulsions, loss of consciousness, impaired coordination of movement (most often these are signs of encephalitis);
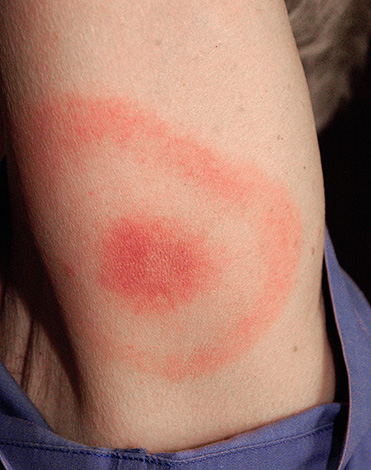
- The appearance of erythema migrans - a large red, constantly expanding ring on the skin around the bite site (this is the most characteristic sign of Lyme disease);
- Nausea;
- Extensive swelling of tissues and (or) severe sudden pain at the site of the bite, even if there are no signs of a bite anymore.
If any of these symptoms appear, you should consult an infectious disease specialist as soon as possible. It is timely treatment started for all tick-borne infections that allows to avoid the threat of severe consequences.
It should be borne in mind that if the site of the bite is swollen and reddened immediately after the extraction of the tick, this does not indicate infection, but is associated only with skin damage and the body’s natural reaction to the parasite entering the saliva tissue.One of the signs of infection is lump retention for more than 4 days with the development of generalized symptoms.
Similarly, if immediately (on the same day) after a bite, a head, arm or leg, for which the parasite has bitten, hurts, then this is hardly associated with an infection. For the development and manifestation of it you need at least a few days, and immediately the symptoms of the disease do not appear.
Even if, when analyzing a tick, it revealed an infection with an infection, the likelihood of developing a disease in a person is small. According to statistics, even with bites from infected ticks, an average of 2-6% of those bitten get sick.
However, the onset of the disease can be diagnosed even in the incubation period. For this you need to pass a blood test for tick-borne encephalitis and borreliosis. An immunoassay in the blood reveals antibodies to the causative agents of the corresponding diseases.
As noted above, such an analysis will be indicative no earlier than 10 days after the bite. On the 14th day after the incident, it makes sense to donate blood for antibodies to tick-borne encephalitis, and after 20 days for antibodies to borrelia. If a disease is confirmed, the doctor will prescribe treatment before the onset of symptoms.
Prevent tick bites
It is easier to prevent a tick bite than to run through hospitals and worry about possible infection. At the same time, all the complexities of such protection against the attacks of bloodsuckers are primarily organizational, not requiring any special knowledge and skills.

Going to a place where you can encounter ticks, you need to dress in such a way that the maximum body area is covered with clothes, even if not dense (the tick cannot bite through clothes - even through thin tights). You should have socks on your feet, you need to tuck in your trousers, and in your trousers - a shirt. In this case, the parasite who had attached itself to the leg would have had to climb to the throat to get under the clothes. Things themselves should be chosen light, on which such a hooked "passenger" will be easy to notice and remove in time.
It is also useful to use repellents based on pyrethroids and DEET. Many of these tools are suitable for children.
In nature, in groups of people, participants need to inspect each other every 2-3 hours and remove the detected ticks. At the same time, special attention is paid to the places of the most frequent attachment of parasites — to the stomach, armpits, groin, chin, behind the ears.

On a note
If the tick has just started to dig in, or is still crawling on the skin in search of a place to suck, it is hardly noticeable, since it has a small size. A small larvae sucked in is also not always easy to detect - it can be similar to papilloma, and even with close inspection it can be “skipped” with a glance. Similarly, it is difficult to find a tick in his hair, if he climbed onto his head.
When going on nature in the endemic region of tick-borne encephalitis, the region must first be vaccinated against CE. Then even a tick bite that happens will be much less dangerous: a person will not get sick with encephalitis, and even if he gets sick (which happens very rarely with vaccination), the disease will proceed easily and without complications.
However, vaccination cannot protect against Lyme borreliosis. A specific anti-borreliosis vaccine has not been developed.
Finally, some insurance companies today offer tick bite insurance. The insurance package for one person costs about 500-800 rubles, and the insurance amount covers the analysis of the tick for encephalitis and borreliosis, blood tests of the bitten and the complete treatment of the disease.
Useful video about first aid for tick bites
What to do if a child is bitten by a tick



